Custom Claims Repricing
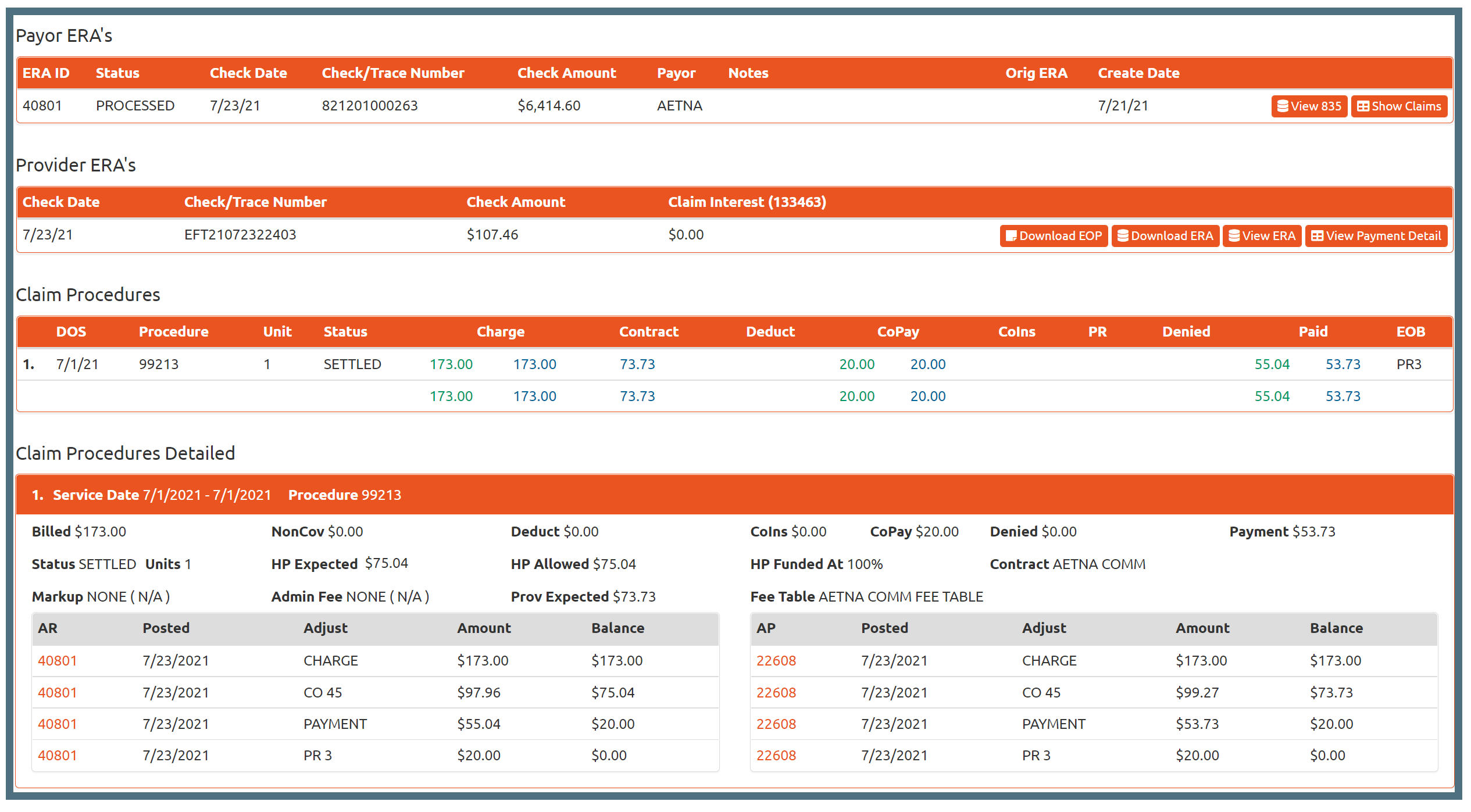
This is an example of a markup/admin fee claim that has a health plan AR component for funding. Notice that the accounts payable (AP) is separate from the accounts receivable (AR). This clear separation of the two accounts allows our system to track a balance between you and the payor and you and the provider.
Many of our clients have a need to price claims based on custom contracts with both the payor and provider. This could be a risk based per member, per month contract or simply a fee for service based contract. Prices for claims are defined when they are received from the provider. Defining what is owed to the provider versus what the payor owes up front means that you can track both sides of your accounting with ease.

React to Payor Updates
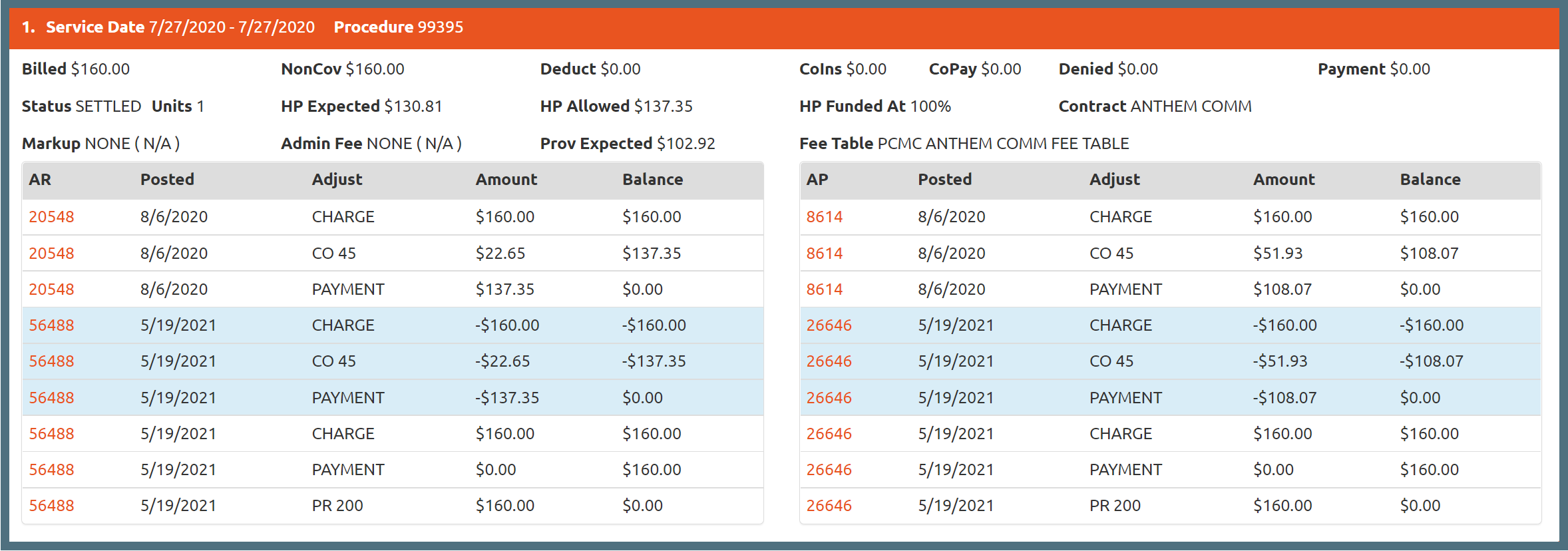

Recoupments and repayments from health plan (AR) are handled automatically on the provider side (AP).
The payor sent this claim originally and it was repriced and paid. Later, the same claim was reversed and denied. Track this progress and clearly see how the AR and AP accounts were separately paid.
Notice how the reversal adjustments (in blue) are also priced to avoid taking too much back from the provider.
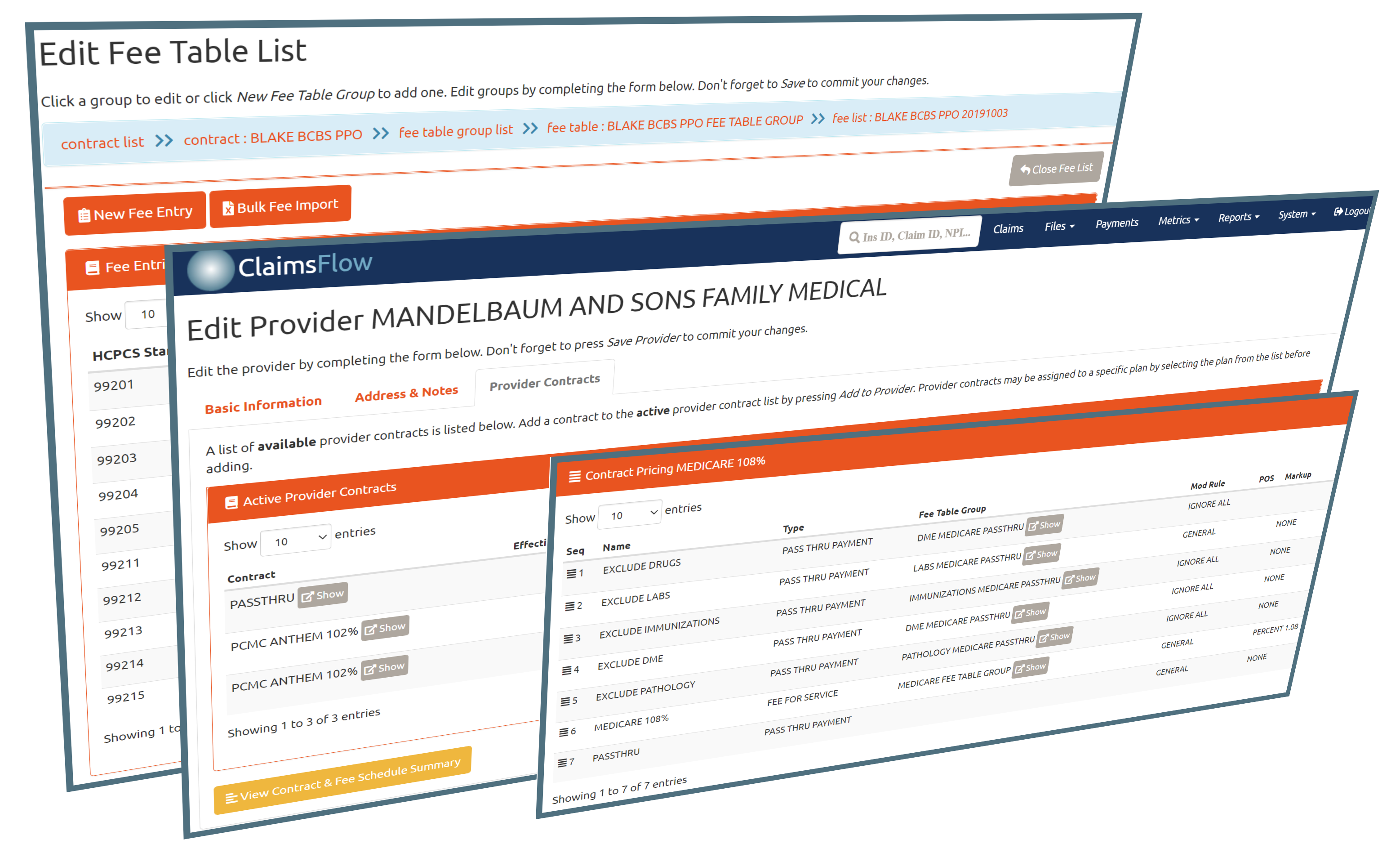
Flexible Contract Management
We create a well-defined set of rules for claims pricing and administration fees. These rules are not limited to static fee schedules. We have the capability to expand the schedule by effective and term dates, percentages, and other custom rules without the need to duplicate large fee tables for any special cases.
The contracts and fee schedules are easily managed using online tools that are able to address these common issues without making a mess of your data. The editors typically support custom contracts for fee-for-service schedules, risk based contracts, bulk import and other special case rules.
Our systems are capable of pricing claims based on DOS, strict contract amounts, billed amounts, or percentages of these amounts. We also have rules designed to handle risk or pass-through claims that need no pricing other than the ability to track what is owed in COB or patient responsibility balances.