X12 ANSI EDI
We have experience creating and parsing ANSI EDI files such as 837, 835, 277 and others. We are able to parse the received claims into the system for tracking and reporting. We then have the ability to take the same claims and automatically build a separate 837 file with your claim/account numbers and contracted pricing. This includes the ability to split, combine, or supplement claims as needed.
It's also possible to automate tasks using data found in 270/271 member status and 276/277 claim status reports from the health plan. These tasks can help resolve issues in a timely manner instead of waiting for a denial in an 835.
Our claim tools can display EDI in a human readable fashion. Easily identify loops and segments in popover text to see how that field is defined. Try clicking a field on the left to view ANSI details for that loop and segment.

Automation
It's common practice to automate the exchange of claims files with a health plan or clearing house. We take this a step further and automate any daily tasks that can be defined by a series of rules.
The schedule is configurable and contains an email notification system so you can easily supervise your automated tasks. This ensures that the health plan is never waiting on you to respond to denials or payments.
Being able to have a centralized place to collect and manage claims files can reduce turn-around times for your claims business. We can also provide this service as an addition to an existing claims or practice management system.
Flexible Contract Management
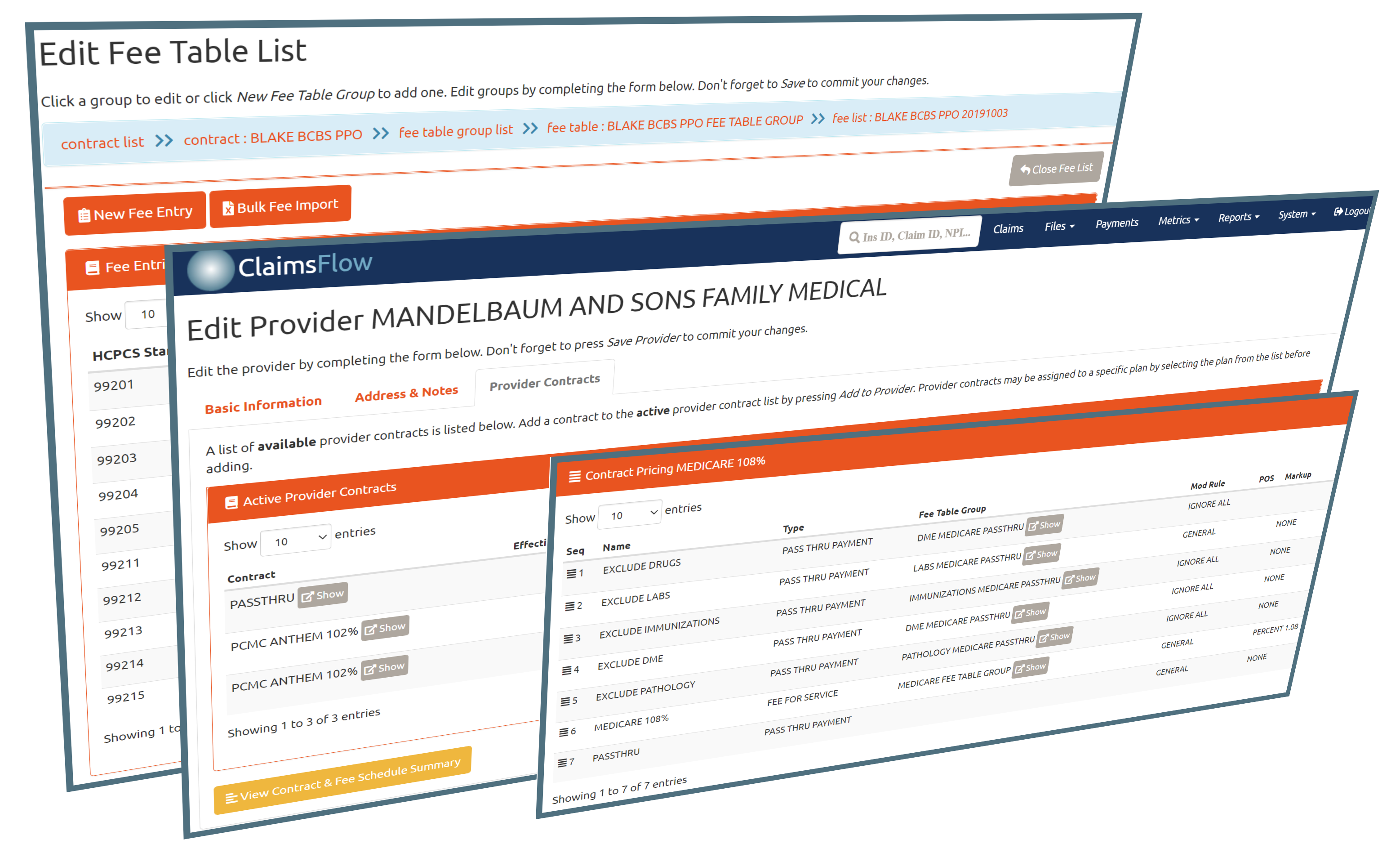
We create a well-defined set of rules for claims pricing and administration fees. These rules are not limited to static fee schedules. We have the capability to expand the schedule by effective and term dates, percentages, and other custom rules without the need to duplicate large fee tables for any special cases.
The contracts and fee schedules are easily managed using online tools that are able to address these common issues without making a mess of your data. The editors typically support custom contracts for fee-for-service schedules, risk based contracts, bulk import and other special case rules.
Our systems are capable of pricing claims based on DOS, strict contract amounts, billed amounts, or percentages of these amounts. We also have rules designed to handle risk or pass-through claims that need no pricing other than the ability to track what is owed in COB or patient responsibility balances.